
Ear, Nose & Throat
A 3 year old girl is brought to the Emergency Department by her worried parents. She has had a fever for 2 days and has been increasingly struggling to tolerate oral fluids. She has no significant past medical history. Due to parental views she has not been immunised. She indicates to her neck when asked "Where does it hurt?". On examination you note a fever, tachycardia and tachypnoea. She is sat forwards and drooling. What is the most likely diagnosis?
Answer:
The child has features of epiglottitis. The typical features of epiglottitis are a rapid onset of pyrexia, sore throat, muffled speech, dysphagia, drooling and stridor. The child usually looks unwell in acute distress; sitting forwards, mouth open, drooling with tongue protruding.Epiglottitis
Ear, Nose & Throat
Last Updated: 14th December 2023
Epiglottitis is a rapidly progressive cellulitis of the epiglottis and adjacent structures that has the potential to cause abrupt and complete airway obstruction.
Infectious agents
Following the introduction of the Haemophilus influenzae type b (Hib) vaccination in 1992, childhood epiglottitis has become rare, and more cases now occur in adults. However, children who are fully immunised can still get Hib culture positive epiglottitis. Other potential pathogens include Streptococcus pneumoniae, Staphylococcus aureus, and MRSA.
Clinical features
There is a rapid onset of pyrexia, sore throat, muffled speech, dysphagia, drooling and stridor. The child usually looks unwell in acute distress; sitting forwards, mouth open, drooling with tongue protruding.
No action should be taken that could stimulate a child with suspected epiglottitis (including examination of the oral cavity, starting intravenous lines, blood draws, or even separation from a parent) unless there are facilities for immediate intubation/tracheostomy because of the possibility of precipitating complete airway obstruction or cardiopulmonary arrest.
Investigations
Diagnosis is made on clinical grounds, and laboratory or other interventions should not preclude or delay timely control of the airway if epiglottitis is suspected.
- Fiberoptic laryngoscopy remains the 'gold standard' for diagnosing epiglottitis, as the epiglottis can be seen directly. Laryngoscopy in these patients should only be performed in areas such as operating theatres which are prepared for intubation or tracheostomy in the event of upper airway obstruction.
- Lateral neck X-ray may be useful if laryngoscopy is not possible. Soft-tissue radiograph of the neck may show the 'thumbprint sign' (See below - left column normal, right column epiglottitis).
- Throat swabs may be taken when the airway is secure, or when intubation/tracheostomy facilities are at hand.
- Blood cultures may be taken if the patient is systemically unwell.
- CT or MRI scans may be performed if abscess formation is suspected.
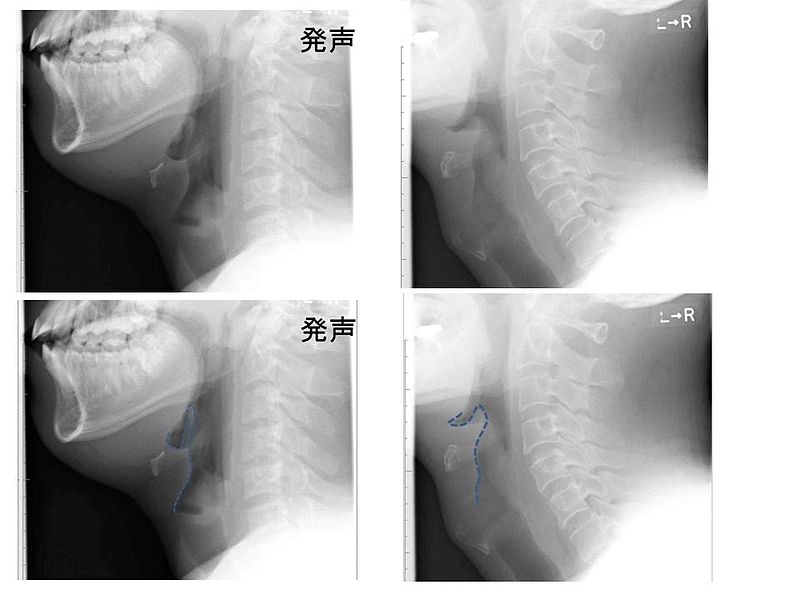
Lateral Neck X-ray Showing 'Thumbprint Sign' in Acute Epiglottitis. (Image by Med Chaos (Own work) [CC BY-SA 3.0 , via Wikimedia Commons)
Management
Management of this condition remains controversial. The cornerstone is not to distress the child as this can precipitate complete airway obstruction.
Oxygen should be administered if the child is hypoxic.
In the first instance, intravenous antibiotics should be administered, if intravenous access can be achieved without distress. Treatment choice is by hospital guideline with a third-generation cephalosporin being a reasonable choice.
Children under 6 years of age require urgent intubation, ideally in theatre by an experienced anaesthetist with an ENT surgeon present. If there is no time to transfer the child to theatre, then a difficult intubation trolley and cricothyroidotomy kit must be ready. In those over the age of 6 years, observation may be an option following consultation with an ENT and PICU consultant.
The average time for children to remain intubated is 48 to 96 hours. Extubation occurs when direct visualisation of the epiglottis confirms that the inflammation of the epiglottis and surrounding tissues has resolved.
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

