
Cardiology
This was previously featured in an exam
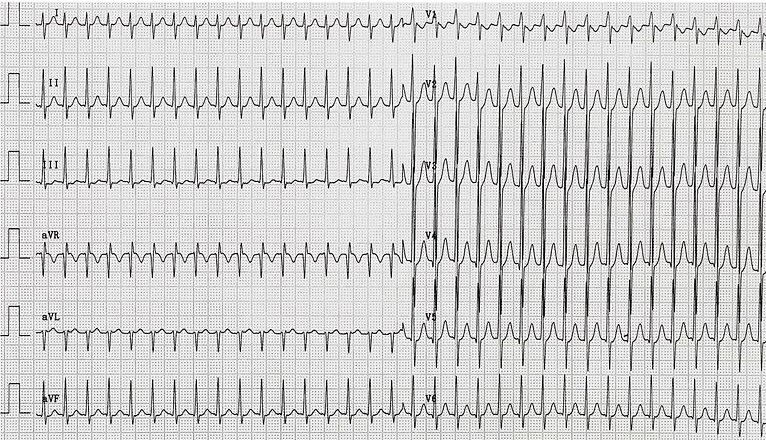
A 34 year old man presents to the Emergency Department after developing palpitations during a 5km race. On examination his heart rate is 185 beats per minute, BP 83/54 and RR 20 breaths per minute. He reports no loss of consciousness, breathlessness or chest pain. He has no significant past medical history. Which of the following treatments is most appropriate for this patient?
Answer:
The ECG and history are consistent with re-entry paroxysmal supraventricular tachycardia (SVT). The patient is hypotensive - this is an "adverse feature" and therefore synchronised DC cardioversion is indicated.Peri-Arrest Arrhythmias
Cardiology
Last Updated: 18th September 2024
Sequence of action in peri-arrest arrhythmias
- ABCDE approach
- Early ECG monitoring
- Identification of adverse features
- Intravenous access
- Oxygen if hypoxia present
- Immediate treatment of arrhythmia
- no treatment needed
- simple clinical intervention (e.g. vagal manoeuvres, percussion pacing)
- pharmacological treatment
- electrical treatment (e.g. cardioversion, pacing)
- Subsequent monitoring and treatment
- Continued ECG monitoring
- Correction of reversible factors
- Expert help and advice
Adverse features
The presence or absence of adverse features will dictate the urgency and choice of treatment for most arrhythmias. The following adverse features indicate that a patient is unstable and at risk of deterioration:
- Shock
- hypotension (SBP < 90 mmHg), pallor, sweating, cold extremities, confusion, impaired consciousness
- Syncope
- transient loss of consciousness due to global reduction in blood flow to the brain
- Heart failure
- pulmonary oedema, raised JVP, peripheral oedema, hepatomegaly
- Myocardial ischaemia
- ischaemic chest pain, ischaemic changes on ECG
Extremes of heart rate can also indicate that a patient is at risk of deterioration:
- Extreme tachycardia
- The faster the heart rate, the less well it will be tolerated. When HR increases, diastole is shortened to a greater degree than systole. The heart doesn't have time to fill properly during diastole thus reducing cardiac output. Coronary blood flow is reduced (because this mostly occurs during diastole) potentially causing myocardial ischaemia.
- Extreme bradycardia
- The slower the heart rate the less well it will be tolerated. This is especially so when people with severe heart disease cannot compensate for the bradycardia by increasing stroke volume.
Management of tachyarrhythmias
For patients with adverse features
Use synchronised cardioversion:
- Under conscious sedation or general anaesthesia
- Ensure defibrillator is set to deliver a synchronised shock (to coincide with the R wave)
- Start with 120 – 150 J for broad-complex tachycardia
- Start with 70 – 120 J for narrow-complex tachycardia or atrial flutter
- For atrial fibrillation (AF) start at maximal defibrillator output
- For AF and atrial flutter use anteroposterior defibrillator pad positions where practicable
- Increase shock energy in increments if initial attempt fails and perform up to three attempts
- If cardioversion fails to terminate the arrhythmia, and adverse features persist, give amiodarone 300 mg IV over 10 – 20 mins and attempt further cardioversion. The loading dose of amiodarone can be followed by an infusion of 900 mg over 24 h, given via a large vein.
For patients without adverse features
Broad-complex tachycardia (QRS ≥ 0.12 s):
- Regular broad-complex tachycardia
- Ventricular tachycardia
- Treat with amiodarone 300 mg IV over 10 - 60 mins, followed by an infusion of 900 mg over 24 h
- If rhythm persists after initial dose of amiodarone, synchronised cardioversion may be considered but such a decision should be deferred to an expert
- Supraventricular tachycardia with bundle branch block
- Treat as for narrow-complex tachycardia if previously diagnosed
- Ventricular tachycardia
- Irregular broad-complex tachycardia
- Atrial fibrillation with bundle branch block (most likely)
- Treat as for irregular narrow-complex tachycardia
- Pre-excited atrial fibrillation (in patients with Wolff-Parkinson-White syndrome)
- Seek expert advice
- Polymorphic ventricular tachycardia (e.g. torsade de pointes)
- Stop QT prolonging drugs, correct electrolyte abnormalities, give magnesium sulphate 2 g IV over 10 mins, obtain expert help, arrange immediate synchronised cardioversion if adverse features develop
- Atrial fibrillation with bundle branch block (most likely)
Narrow-complex tachycardia (QRS < 0.12 s):
- Regular narrow-complex tachycardia
- Sinus tachycardia
- Do not attempt to treat sinus tachycardia with cardioversion or anti-arrhythmic drugs
- Paroxysmal supraventricular tachycardia (SVT)
- Atrioventricular nodal re-entry tachycardia, AVNRT (most common type)
- Atrioventricular re-entry tachycardia, AVRT (due to WPW syndrome)
- Atrial flutter with regular AV conduction (usually 2:1)
- Treatment of narrow-complex tachyarrhythmia
- Start with vagal manoeuvres (may reveal atrial flutter)
- Carotid sinus massage
- Valsalva manoeuvre
- If arrhythmia persists and is not atrial flutter, give adenosine
- Give 6 mg rapid IV bolus in large vein (warn patient they will feel unwell)
- Record ECG during injection
- If ventricular rate slows transiently and then speeds up again, look for atrial activity, such as atrial flutter or other atrial tachycardia and treat accordingly
- If there is no response – give a 12 mg bolus, and one further 18 mg bolus if still no response
- Vagal manoeuvres or adenosine will terminate almost all AVNRT or AVRT within seconds, failure to terminate suggests an atrial tachycardia such as atrial flutter
- If adenosine is contraindicated or fails, consider giving verapamil 2.5 – 5 mg IV over 2 minutes or a beta-blocker such as metoprolol (2.5-15 mg given IV in 2.5 mg bolus doses)
- If the narrow-complex tachycardia persists, consider synchronised cardioversion
- Start with vagal manoeuvres (may reveal atrial flutter)
- Sinus tachycardia
- Irregular narrow-complex tachycardia
- Atrial fibrillation with rapid ventricular response (most likely)
- Consider rate or rhythm control, assess thromboembolic risk and consider anticoagulation
- Atrial flutter with variable AV conduction
- Control rate e.g. beta-blocker
- Atrial fibrillation with rapid ventricular response (most likely)
Management of bradyarrhythmias
For patients with adverse features
- Give atropine 500 mcg IV and if necessary repeat every 3 – 5 minutes to a total of 3 mg.
- If bradycardia with adverse features persists despite atropine, consider cardiac pacing.
- If pacing cannot be achieved promptly, consider the use of second line drugs. Seek expert help to select the most appropriate choice.
- In some clinical settings second-line drugs may be appropriate before the use of cardiac pacing. For example:
- Consider giving intravenous glucagon if a beta-blocker or calcium-channel blocker is a likely cause of the bradycardia.
- Consider using digoxin-specific antibody fragments for bradycardia caused by digoxin toxicity.
- Consider using aminophylline for bradycardia complicating acute inferior wall myocardial infarction, spinal cord injury or cardiac transplantation.
- Other options for second-line drug therapy include infusion of isoprenaline, adrenaline or dopamine.
For patients without adverse features
- In a patient with no adverse features and no high risk of progression to asystole, do not initiate immediate treatment, continue to monitor the patient and assess them to identify the cause of the bradycardia, treat reversible causes and seek expert help with further assessment and treatment
- In a patient with no adverse features but with a high risk of progression to asystole, treat as for patients with adverse features
- Risk of asystole:
- Recent asystole
- Mobitz type II AV block
- Complete heart block with broad QRS
- Ventricular pause > 3 s
Torsade de Pointes (TdP)
TdP is an uncommon and distinctive form of polymorphic ventricular tachycardia (VT) characterised by a gradual change in the amplitude and twisting of the QRS complexes around the isoelectric line. TdP is associated with a prolonged QT interval, which may be congenital or acquired. TdP usually terminates spontaneously but frequently recurs and may degenerate into ventricular fibrillation.
Management of TdP:
- Stop QT prolonging drugs
- Correct electrolyte abnormalities
- Give magnesium sulphate 2 g IV over 10 mins
- Obtain expert help
- Arrange immediate synchronised cardioversion if adverse features develop
Wolff-Parkinson-White (WPW) syndrome
- WPW syndrome is a recognised but rare cause of sudden cardiac death (SCD). The existence of an atrioventricular accessory pathway in this syndrome results in ventricular preexcitation, which appears with short PR interval, wide QRS complex, and delta wave on ECG. The refractory period in the anterograde direction of accessory pathway determines the ventricular rate in the setting of atrial fibrillation and WPW. Most patients with WPW syndrome and SCD develop atrial fibrillation with a rapid ventricular response over the accessory pathway, which induces VF.
- Symptomatic patients should be treated by antiarrhythmic medications (e.g. procainamide), catheter ablation of the accessory pathway, or electrical cardioversion depending on the severity and frequency of symptoms. Asymptomatic patients may be observed without treatment.
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

