.png)
Procedural Skills (SLO6)
A 42 year old man presents to ED complaining of a headache and a fever. A lumbar puncture is performed and the results show:
- WCC 460 cells x 106/L
- Predominant cell type: Lymphocytes
- Glucose 1.3 mmol/L
- Protein 1.2 g/L
- India ink staining after the culture is negative
What is the most likely diagnosis?
Answer:
The glucose is low, indicating excessive glucose consumption, which rules out viral meningitis. The predominance of lymphocytes suggests a more chronic infection and rules out bacterial meningitis. The negative India ink stain rules out cryptococcal meningitis. Finally, the extremely large number of lymphocytes and amount of protein make tuberculosis more likely than malignant meningitis. Ziehl–Neelsen staining or PCR would confirm the diagnosis.Lumbar Puncture
Procedural Skills (SLO6)
Last Updated: 13th March 2021
Indications
- To evaluate intracranial pressure and CSF composition
- Suspected meningitis
- Suspected subarachnoid haemorrhage
- Suspicion of CNS disease e.g. malignancy, idiopathic intracranial hypertension, infection or inflammation, demyelinating conditions
- To therapeutically reduce intracranial pressure e.g. idiopathic intracranial hypertension
- To administer intrathecal medications e.g. chemotherapy
Contraindications
- Infection at puncture site
- Anticoagulants or bleeding diathesis
- Increased intracranial pressure
- If papilloedema or focal neurologic deficits are present, CT or MRI should be done before lumbar puncture to rule out presence of a mass that could precipitate transtentorial or cerebellar herniation
Clinical anatomy
In adults, the spinal cord typically ends between L1/L2 whereas the subarachnoid space extends to approximately the lower border of vertebra S2. As a result of this, CSF can be withdrawn from the subarachnoid space in the lower lumbar region without endangering the spinal cord. Lumbar puncture is usually performed in the intervertebral space L4/L5 or L3/L4 (at the same height as the iliac crest).
When performing a lumbar puncture, the needle passes between adjacent vertebral spinous processes, through the supraspinous and interspinous ligaments and through the ligamentum flavum to enter the extradural space. The needle then continues through the dura and the arachnoid mater to enter the subarachnoid space.
Layers penetrated during lumbar puncture:
- Skin
- Superficial fascia
- Supraspinous ligament
- Interspinous ligament
- Ligamentum flavum (first 'give')
- Extradural space
- Dura mater (second 'give')
- Subdural space
- Arachnoid mater
- Subarachnoid space (containing CSF)
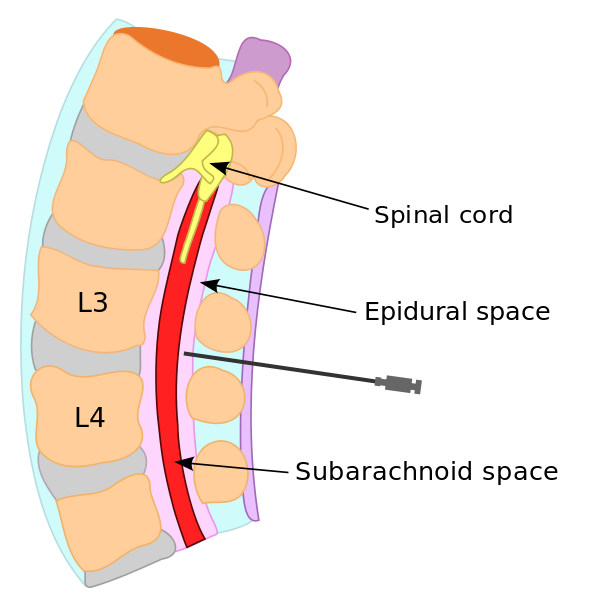
Lumbar Puncture. (Image by Gurch [Public domain], via Wikimedia Commons)
Procedure
- For the procedure, the patient is typically in the left lateral decubitus position. A cooperative patient is asked to hug the knees and curl up as tightly as possible so as to open the interlaminar spaces. Assistants may have to hold patients who cannot maintain this position, or the spine may be flexed better by having patients, particularly obese patients, sit on the side of the bed and lean over a bedside tray table. If the procedure is performed with the patient in the sitting position and an opening pressure is required, replace the stylet and have an assistant help the patient into the left lateral recumbent position.
- The skin is washed with iodine, then wiped with alcohol to remove the iodine and prevent its introduction into the subarachnoid space.
- Local anaesthetic is administered first to the skin and then to the deeper tissue; the needle is inserted to its hub, aspirated to confirm that it is not in a blood vessel and local anaesthetic injected as the needle is withdrawn; this process is repeated above, below and to the sides very slightly, so that if redirection of the spinal needle is necessary, the area will still be anaesthetised.
- A lumbar puncture needle with stylet is inserted into the L3/L4 or L4/L5 interspace (the L4 spinous process is typically on a line between the posterior-superior iliac crests); the needle is aimed rostrally toward the patient’s umbilicus and always kept parallel to the floor. The bevel is oriented parallel to the longitudinal dural fibers to increase the chances that the needle will separate the fibers rather than cut them; in the lateral recumbent position, the bevel should face up, and in the sitting position, it should face to one side or the other.
- Entrance into the subarachnoid space is often accompanied by a discernible pop. Otherwise, the stylet should be withdrawn after approximately 4-5 cm and observed for fluid return. If no fluid is returned, the stylet should be replaced, the needle advanced or withdrawn a few millimeters, and fluid return rechecked. This process is continued until fluid is successfully returned.
- For measurement of the opening pressure, the patient must be in the lateral recumbent position. After fluid is returned from the needle, the manometer is attached through the stopcock, and the height of the fluid column noted. The patient’s legs should be straightened during the measurement of the open pressure, or a falsely elevated pressure will be obtained.
- The 4 tubes are each filled with about 2 to 10 mL of CSF for testing. If possible, the CSF that is in the manometer should be used for tube 1.
- The stylet is then replaced, and the needle removed. A sterile dressing is applied, and the patient placed in the supine position.
Complications
- Post-LP headache (most common complication)
- Bloody tap
- Dry tap
- Infection
- Bleeding
- Dysaesthesia
- Cerebral herniation (rare but potentially fatal)
CSF interpretation
- Physical characteristics
- Opening pressure: normally 10 - 20 cm H2O, may be elevated in infection or bleeding
- Colour: clear and colourless is normal
- Turbidity: cloudy or turbid CSF may indicate the presence of WBCs, RBCs, microorganisms or an increase in protein levels
- Viscosity: ‘thick’ CSF may be seen in infection
- Bloody: bloody fluid may indicate a traumatic puncture or subarachnoid haemorrhage
- Biochemistry
- CSF glucose: usually about 2/3s that of serum glucose, may be decreased in bacterial or TB infection but usually remains normal in viral infection
- CSF protein: increase in protein may be seen in infection, spinal cord tumour or bloody puncture (special examinations for globulin, oligoclonal banding and myelin basic protein aid in diagnosis of a demyelinating disorder)
- CSF lactic acid: usually raised in bacterial infection, but normal in viral infection
- CSF lactate dehydrogenase (LDH): usually raised in bacterial infection, but low or normal in viral infection
- CSF xanthochromia (bilirubin): seen following subarachnoid haemorrhage
- Microscopy
- CSF RBC count: presence of red blood cells may indicate bleeding into the CSF or a ‘traumatic tap’
- CSF WBC count: raised in infection or inflammation of the CNS
- CSF WBC differential: neutrophils increased in bacterial infection, an increase in lymphocytes with viral or TB infection
- Microbiology
- Stains
- Bacteria (Gram stain)
- TB (acid-fast stain or immunofluorescence)
- Cryptococcus sp (India ink)
- CSF culture and sensitivity
- CSF viral PCR testing
- Other specific tests depending on which organisms are suspected
- Stains
Differentiating between aetiology of meningitis
| CSF Analysis | Normal | Bacterial | Viral | TB |
|---|---|---|---|---|
| Appearance | Clear and colourless | Turbid | Normal | Fibrin web |
| WCC (mm3) | 0 - 5 | High | High | High |
| Predominant cell type | - | Neutrophils | Lymphocytes | Lymphocytes |
| Glucose (mmol/L)
CSF:Serum Ratio |
2.5 - 4.4
0.6 |
Low | Normal | Low |
| Protein (g/L) | 0.2 - 0.4 | High | Normal or High | High |
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

