.png)
Procedural Skills (SLO6)
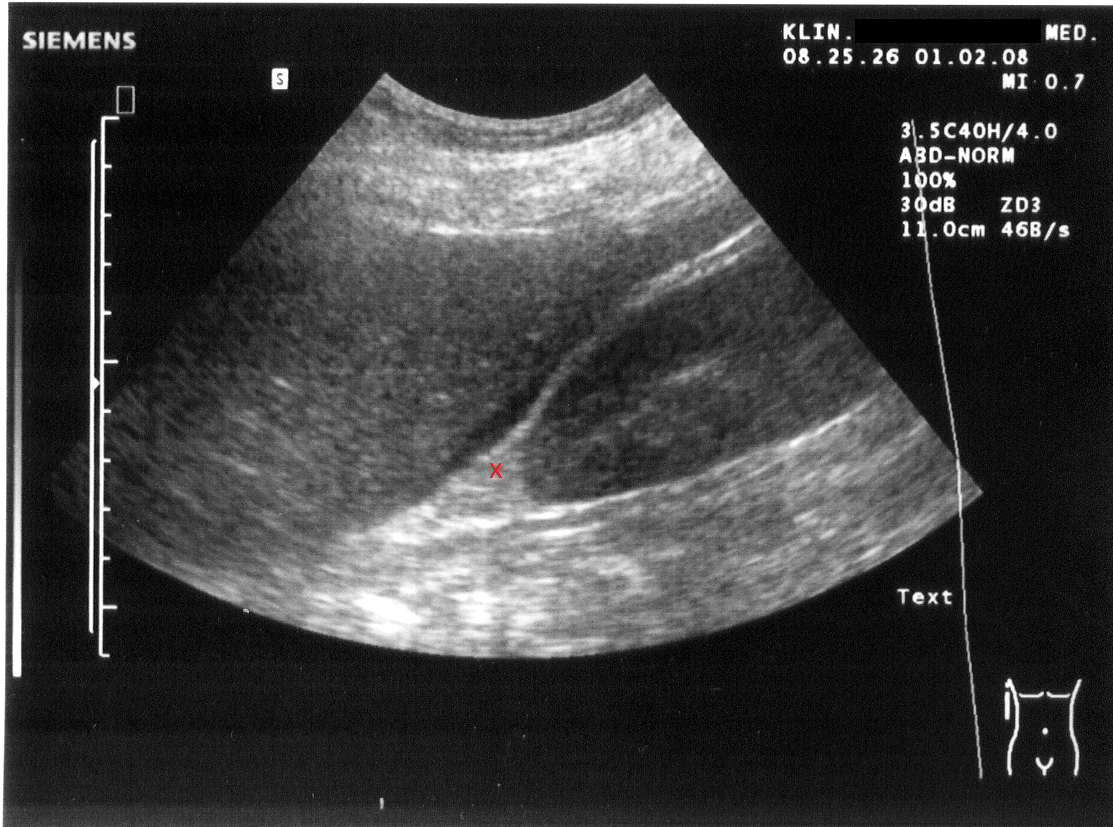
You are participating in a simulation session for Focused Assessment with Sonography for Trauma (FAST). An image of the abdomen is shown. What is the label X depicting?
Answer:
Morison's pouch is the area between the liver and the right kidney. It's also called the hepatorenal recess or right subhepatic space.Focused Assessment with Sonography for Trauma (FAST)
Procedural Skills (SLO6) / Trauma
Last Updated: 8th September 2022
The focused assessment with sonography in trauma (FAST) examination is a non-invasive point-of-care test whose role is to guide clinical decision making and direct angiographic or surgical interventions. It can be used by clinicians to diagnose haemopericardium or haemoperitoneum secondary to clinically significant injuries on ultrasound (US).
FAST is no substitute for CT and a more definitive assessment of the patient is obtained with CT. Indeed, a positive FAST scan in a stable patient should always lead to a CT scan. However, a positive FAST scan in an unstable patient may lead to immediate laparotomy.
Advantages of FAST
- Can be performed rapidly within 3 - 4 minutes
- Performed at bedside thereby avoiding the risks associated with transport
- Non-invasive and does not involve the use of ionising radiation
- Can be performed on an unstable patient (whereas a CT requires the patient to be stable)
- May be repeated as many times as necessary
- High specificity therefore usually accurate for identifying injury when positive (BUT lower sensitivity therefore cannot be used to rule out injury when negative)
Disadvantages of FAST
- Operator-dependent
- Can miss small amounts of intraperitoneal bleeding (requires minimum of 100-200 ml of fluid for visualisation)
- Bowel gas and subcutaneous air distort images
- Can miss diaphragm, bowel, and pancreatic injuries
- Does not completely assess retroperitoneal structures
- Does not visualise extraluminal air
- Body habitus can limit image clarity
NICE recommendations for FAST/eFAST in major trauma
- Imaging in haemorrhage (in-hospital setting)
- Imaging for haemorrhage in patients with suspected haemorrhage should be performed urgently, and the images should be interpreted immediately by a healthcare professional with training and skills in this area.
- Limit diagnostic imaging (such as chest and pelvis X-rays or FAST) to the minimum needed to direct intervention in patients with suspected haemorrhage and haemodynamic instability who are not responding to volume resuscitation.
- Be aware that a negative FAST does not exclude intraperitoneal or retroperitoneal haemorrhage.
- Consider immediate CT for patients with suspected haemorrhage if they are responding to resuscitation or if their haemodynamic status is normal.
- Do not use FAST or other diagnostic imaging before immediate CT in patients with major trauma.
- Do not use FAST as a screening modality to determine the need for CT in patients with major trauma.
- Imaging in chest trauma (in-hospital settings)
- Imaging for chest trauma in patients with suspected chest trauma should be performed urgently, and the images should be interpreted immediately by a healthcare professional with training and skills in this area.
- Consider immediate chest X-ray and/or eFAST as part of the primary survey to assess chest trauma in adults (16 or over) with severe respiratory compromise.
- Consider immediate CT for adults (16 or over) with suspected chest trauma without severe respiratory compromise who are responding to resuscitation or whose haemodynamic status is normal.
- Consider chest X-ray and/or ultrasound for first-line imaging to assess chest trauma in children (under 16s).
- Do not routinely use CT for first-line imaging to assess chest trauma in children (under 16s).
How to perform FAST
- Use a low-frequency probe (3.5 mHz).
- The marker on the probe should always be orientated towards the patient’s head, or to their right (except in the long axis parasternal view).
- Cardiac view:
- Start with the heart to ensure the gain is set appropriately.
- Fluid within the heart will appear black.
- Place the probe in the subxiphoid space, with the probe marker to the right.
- The probe angle is shallow, and the liver is used as an acoustic window.
- Alternatively try the parasternal view; in this instance, the marker should point down to the heart apex to gain a standard view.
- Right upper quadrant (RUQ) view (includes Morrison's pouch and the right costophrenic pleural recess):
- Place the probe marker toward the head in the coronal plane in the anterior axillary line.
- Rotate the probe obliquely and scan from cephalad to caudad to visualise the diaphragm, liver, and kidney.
- Left upper quadrant (LUQ) view (includes splenorenal recess and the left costophrenic pleural recess):
- Position the probe marker toward the head in the coronal plane.
- Begin scan more cephalad than on the right and more posterior.
- Begin in the midaxillary line.
- Rotate the probe obliquely and visualise the diaphragm, spleen, and kidney.
- Pelvic view (includes the rectovesical pouch in males and the pouch of Douglas in females):
- Ideally, the bladder is full.
- Place the probe above the pubic bone with the probe marker pointing to the right and scan for fluid appearing as a dark stripe.
- Rotate the probe 90 degrees so the probe marker points to the head and scan again for fluid.
Identifying free fluid
- On the pericardial view, look for a black stripe of fluid separating the hyperechoic pericardium from the grey myocardium. This stripe represents fluid.
- Look at the hepatorenal space. Intraperitoneal fluid has a black hypoechoic or anechoic appearance.
- Look at the splenorenal space. Blood will appear as a hypoechoic or anechoic strip in this area.
- Look around the bladder for an area of hypoechogenicity.
- If no free fluid is seen, consider a repeat scan, perhaps 10 minutes later. If at any stage a black line anterior to the renal capsule, or black area in the pleural recess is present, the interpretation should be that there is free fluid present. Be sure you have thoroughly visualised all spaces before declaring an examination negative.
- N.B.
- The RUQ is the area where free fluid is likely to be detected first; early peritoneal collections are seen just anterior to the renal capsule and appear as a black stripe.
- The LUQ view requires the probe to be slightly higher, i.e. toward the axilla, than the RUQ view.
- The pleural space can be visualised in the RUQ and LUQ views. Small pleural collections and pericardial collections begin to accumulate posteriorly.
- A small amount of fluid in the pouch of Douglas in the female pelvis may be normal following ovulation.
Extended Focused Assessment using Sonography in Trauma (eFAST)
The extended FAST includes the additional evaluation of the anterior and lateral pleural spaces to evaluate for pneumothorax or pleural fluid, presumed to be a haemothorax until proven otherwise in the setting of trauma. A scan is deemed positive if any free fluid is visualised. However, it is important to note that a negative scan does not rule out internal bleeding. The discovery of a lung point where there is a transition from lung sliding is diagnostic of a pneumothorax.
Indications for eFAST include:
- Haemodynamically unstable blunt abdominal trauma
- Haemodynamically stable blunt chest trauma
- Any penetrating trauma to the chest
The FAST exam is less sensitive in the setting of penetrating trauma than blunt trauma due to air in the peritoneal or pleural spaces. Air does not allow ultrasound to penetrate deeper tissue.
Thoracic view:
- Orient the probe in the longitudinal plane with the marker towards the patient’s head.
- Place the probe along the midaxillary region at the level of the 3rd or 4th intercostal space.
- Ensure that ribs are present on the left and right of the ultrasound field.
- Ensure pleura visualised is below the ribs as subcutaneous emphysema can lead to misinterpretation of the true pleural line.
- If there is doubt about pleural sliding, reduce gain until only the pleural line is visible. This allows any movement in the pleural line to be noticed.
- The linear probe can be used to further interrogate the pleural line.
- Switch to M-Mode if required to visualise the interface between the pleura and lung.
- Assess for lung sliding, comet-tail artefacts, seashore sign, barcode sign and/or the presence of a “lung point” to evaluate for pneumothorax.
- Repeat the above technique on the other side of the chest.
Echocardiography in Life Support (ELS)
ELS is learned alongside FAST. It is a limited echocardiogram used in the setting of non-shockable cardiac arrest rhythms (PEA and asystole). The heart is examined during the rhythm check for wall motion and for treatable causes of cardiac arrest. During this short window, the probe is often set to maximum depth and increased gain, to increase the likelihood of locating the heart rapidly. If the heart cannot be seen during the rhythm check, the probe should be removed and CPR resumed immediately.
Assessment includes looking for fluid in the pericardial space, looking for the presence/absence and character of ventricular wall motion, and looking for gross abnormalities of right and left ventricular size. The subxiphoid view is primarily used, augmented by a further view; most commonly the parasternal long axis view. In addition, the longitudinal subxiphoid view allows visualisation of the IVC for assessment of diameter and collapsibility.
ELS has two priorities:
- To assess cardiac movement (and aid decision making in cardiac arrest):
- If there is no cardiac movement
- If the heart is motionless and this corresponds with asystole on the monitor, survival is highly unlikely.
- If there is cardiac movement with sinus rhythm on the monitor
- If the carotid pulse is absent, the patient has 'pseudo-PEA' in which there is mechanical action of the heart, but insufficient magnitude to generate a pulse - survival is much higher in these patients.
- If there is visible ventricular fibrillation
- Some patients thought to be in asystole have been found to have VF on echo - such patients require cardioversion.
- If there is no cardiac movement
- To identify remediable pathology:
- Pericardial effusion large enough to cause cardiac tamponade
- Massive pulmonary embolism (visible thrombus in the heart, right ventricle diameter to left ventricle diameter ratio of greater than one, and a dilated IVC)
- Hypovolaemia (collapsed and small diameter IVC)
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

